Hyperbaric Oxygen Info - Featured article.
HYPERBARIC OXYGEN TREATMENT : THE LAST FRONTIER

Philip B James MB ChB, PhD, DIH, FFOM. Wolfson Hyperbaric Medicine Unit, Ninewells Hospital and Medical School, Dundee, Scotland UK.
Very few innovations have relevance across the many specialist boundaries which now divide the discipline of Medicine, but intravenous - I.V. - fluid therapy is one notable example. Oral fluids are not readily absorbed in shock because, in order to preserve the blood supply to the most vital organs, the blood supply to the gut is greatly reduced. Asked to guess when intravenous fluid therapy was first used, most would suspect it was in the twentieth century, but it was actually in 1832. Two physicians in Leith near Edinburgh, Dr. Thomas Latta and Dr. Robert Lewins, used intravenous saline to save the lives of sixteen of their patients with cholera. Their action was prompted by an article in the Lancet that year by Dr OShaughnessy, a Dublin trained physician, on the importance of electrolytes in blood. Dr. Latta wrote to the Lancet giving an account of the miraculous recovery of the first patient treated with intravenous fluid.
She had apparently reached the last moment of her earthly existence and now nothing could injure her - indeed so entirely was she reduced that I feared that I would not be able to get my apparatus ready ere she expired. Having inserted a tube into the basilic vein, cautiously, anxiously, I watched the effects; ounce after ounce was injected, but no visible change was produced. Still persevering, I thought she began to breathe less laboriously, soon the sharpened features and sunken eye and fallen jaw, pale and cold, bearing the manifest impress of deaths signet, began to glow with returning animation; the pulse, which had long ceased, returned with full vigour to the wrist; at first small and quick, by degrees it became more and more distinct, fuller, slower and firmer and, in the short space of half an hour, when six pints had been injected she expressed in a firm voice that she was free from all uneasiness....
Dr OShaughnessy reading of this success was delighted and wrote to the Lancet:
The results of the practice described by Drs Latta and Lewins exceed my most sanguine anticipations. When we consider that no practitioner would dare to try so novel an experiment, except in cases beyond hope of relief by any ordinary mode of treatment, and, consequently, desperate to the last degree, even a solitary instance of recovery affords matter for congratulation.
An editorial in the same issue compared the new therapy, which simply adds water to the circulation to the workings of a miraculous and supernatural agent. Despite this, it was sixty years before the technique was used again and doctors were still arguing about the need for intravenous fluids in shock during the Second World War. A surgical colleague remembered the intense polarization of the profession that accompanied this debate. Half the profession said that intravenous fluid was life saving in shock, whilst the other half said that it killed patients. To introduce liquid into a vein to rapidly expand the circulation requires increased pressure and so can justifiably be described as hyperbaric water supplementation inviting a comparison with using an increase in atmospheric pressure to deliver more oxygen.
It is necessary to have distrust of the miraculous in Medicine, especially when, for example, claims are made for drugs whose pharmacology and benefit have not been scientifically established. Although oxygen hardly falls into this category as no one seriously denies its importance to life, it is surprising that using a simple enclosure to allow the delivery of high level of oxygen to relieve an acute deficiency is still regarded by some physicians as quackery. They commonly argue that as blood is virtually saturated with oxygen breathing air, no more can be carried, but the saturation referred to is of haemoglobin not plasma and the haemoglobin value can be 100% when the brain is dying from hypoxia. In fact, there is actually no limit to the amount of oxygen which can be carried in plasma and, at three times atmospheric pressure, sufficient can be dissolved to support life without the presence of haemoglobin. Few physicians will be aware of the paper Life without blood giving the details of the experiments which was published in 1959 by Boerema et al, or that the finding has been used many times to save the lives of patients who have refused blood transfusion on religious grounds.
Because of the wide applications of hyperbaric oxygen therapy it is viewed as a panacea, despite the oxygen used being just the same as the oxygen in air, but oxygen, because of its primary importance to metabolism, is a panacea for all the tissues of the body. Fortunately there is no need for patients to be encouraged to breathe because it is automatic, but how often is it remembered that breathing is so essential to recovery in every disease? John Scott Haldane, who can be regarded as the father of oxygen therapy and devised the first apparatus to deliver 100% oxygen stated in 1922 in his book Respiration,
Lack of oxygen not only stops the machine, but also wrecks what we take to be the machinery.
It is possible to survive for a considerable time without food, or even water, but, without sufficient oxygen, survival of critical tissues, such as the brain may be measured in minutes. For there to be any possibility of preventing permanent damage in some neurological conditions, for example, stroke, a successful therapy has to be used within hours. Emergency treatment is universally accepted in heart attacks because it is obvious that if a patient dies from cardiac arrest even the most advanced coronary care is rendered impotent. But the same urgency has yet to be recognized in neurological diseases. The fundamental problem addressed by oxygen at the high dosages possible under hyperbaric conditions, is the rapid correction of oxygen deficiency in the tissues. The principle is simple: the faster hypoxia is corrected, the less likely there is to be permanent damage. Imagine a patient who has been strangled and arrives at a hospital blue and close to death. The question to be answered is direct and simple...
Should the lack of oxygen in such a patient be relieved by giving a low dosage of oxygen over a long period as is presently used, or a large dose immediately?
The answer is obvious, but currently oxygen is simply given to restore normal levels in the blood, which, ironically, is one tissue remarkably resistant to lack of oxygen. However, it is self -evident that having the correct level in the blood does not mean that the tissues have enough. Today, despite dramatic advances in life support clinicians around the World constantly accept the limitation imposed by barometric pressure not realizing that a simple piece of equipment can dramatically alter the outcome. The correction of an acute deficiency of oxygen, like the rehydration of a cholera victim, can be miraculous. Two examples dramatically illustrate the principle and the facts are as relevant now as when they were reported. Unfortunately, many clinicians today would hide behind a dismissal of the cases as mere anecdotes.
In 1965 a patient of Mr. J. R. Belcher at the London Chest Hospital underwent surgery for severe mitral valve disease. He was 50 years old and had been breathless on exertion for 20 years. Deteriorating rapidly and regularly coughing up blood, open heart surgery was very much a last resort. Cardiopulmonary bypass was not yet available and, after opening the chest and the pericardium, an incision was made through the wall of the left ventricle without arresting the heart. The stenosed mitral valve leaflets were freed by the use of a scalpel blade attached to the tip of the surgeons finger.
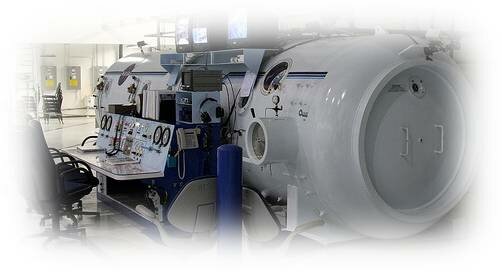
After the operation the patient displayed all the signs of a low cardiac output - failure to recover consciousness with no localising cerebral signs, severe peripheral cyanosis and a very slow capillary refill in the limbs. In an attempt to lower the pulmonary vascular resistance and raise the cardiac output, he was artificially ventilated with 100% oxygen. This was ineffective, and the patient's death seemed certain. Since the patients condition was now desperate, it was decided to use hyperbaric oxygen therapy. He was placed in the Vickers mobile chamber at a pressure of 2 atmospheres absolute. Since there were no facilities in the chamber for artificial respiration, transfusion or drainage these had to be discontinued. The patient's condition began to improve after an hour inside the chamber; he was taken out of it every 2 hours to aspirate from his bronchial tree the considerable amount of heavily bloodstained sputum. After 12 hours treatment, he began to move and gradually recovered consciousness for the first time since the operation.
Despite the patient requiring a ventilator it was disconnected and astonishingly, as the pressure was increased to twice normal atmospheric pressure in the chamber (2 atm abs), he began to breathe in the pure oxygen atmosphere and his colour improved. When he was removed after about two hours for the aspiration of blood from the chest, he rapidly became cyanosed and ventilation on 100% oxygen was reinstituted. Because of further deterioration to the point where death was again imminent with a systolic blood pressure of only 50 mm Hg, he was put back into the chamber and began to breathe spontaneously. Altogether he spent 18 hours out of 24 in the chamber and even required a further six hours of hyperbaric oxygen therapy after another surgical procedure to control intra-thoracic bleeding. He went on to make a full recovery.
Although the article in the Lancet gives the full clinical details, it omits to state a remarkable fact. The patient was not actually treated in the hospital; he was treated in the car park. The company then manufacturing single person (monoplace) chambers, Vickers Medical Ltd., had equipped an ambulance with a chamber and made it available for emergencies. The surgeons as a desperate last measure had asked for the chamber to be brought to the hospital and the patient was treated in the rear of the ambulance by the chief engineer of Vickers Medical, the late Mr John Hounsell. The first author of the paper, Magdi Yacoub, now Sir Magdi Yacoub, has been one of the leading cardiac surgeons in the UK and the paper occupies two pages in the Lancet of March 13th 1965. However such is the lack of understanding of oxygenation that even doctors familiar with hyperbaric conditions would argue that the patient was not fit to go under pressure. We are, of course, all under pressure, the pressure of the Earths atmosphere, which exerts one pound of force per square inch or 1 kilogram for every square centimetre of our body surface area.
The second story is just as dramatic and relevant and the paper was published in the British Medical Journal of 2nd November 1968. It records that at 6.50 pm on January the 16th 1967, an expectant mother, who had been admitted to a hospital in Glasgow for bed rest after a minor ante-partum hemorrhage, complained of the sudden onset of left-sided pins and needles and a severe headache. Within minutes she lapsed into coma with stertorous breathing and rapidly deepening cyanosis. Attempts to achieve adequate oxygenation using 100% oxygen and ventilation were unsuccessful. Several special investigations were undertaken and 24 hours post-onset, faced with a grossly irregular and rapid fetal heart rate, it was decided to undertake a Caesarian section in the large hyperbaric chamber installed in the Western Infirmary, Glasgow. to save the baby. The authors wrote:
Before compression the patient began to have generalized convulsions, which became continuous within minutes and her general condition deteriorated until death was thought to be imminent.... Following compression to 2 atm abs there was a marked improvement in the patients condition: the blood pressure rose to 100/70 mm Hg and the periphery became warm and pink... The fetal heart rate, which had been 200 and irregular immediately before compression, fell to 165 and became regular. Caesarian section was now performed (Professor Ian Donald) and proceeded remarkably smoothly, though it was noted that the uterus remained slightly cyanosed, in spite of the high maternal arterial oxygen tension. A normal live female child was born with an Apgar score of 9.
Sadly the mother had no further treatment and died two and a half months later. The diagnosis, made later, was a cardiomyopathy of pregnancy, but the symptoms point clearly to amniotic fluid embolism, especially as the protein content of the cerebrospinal fluid was found to be 240 mg/100 ml.
As OShaughnessy stated, physicians use new approaches as a last resort. In both these cases, death was close, imdeed seemingly inevitable but only because hyperbaric chambers were available could more oxygen be given. With the catastrophic cascade of events that follow acute oxygen deficiency this was wholly appropriate. Patients treated today using conventional methods die because there is simply no alternative to increasing the pressure and the available oxygen to relieve severe hypoxia. It is little wonder that giving more oxygen is an emotive issue.
The last frontier is an appropriate description for this crucial innovation. The technology is not new - all commercial aircraft today are pressurized - in fact, the first recorded instance of the use of hyperbaric oxygen therapy is reported in the Lancet for 1887. If it were new then it would be easier to introduce today, because the technology is available such as Magnetic Resonance Spectroscopy to demonstrate lack of oxygen objectively. These general innovations in Medicine share predictable features. The profession is divided into believers and non believers. Overstatement is found in both positions. After initial enthusiasm the protagonists, many of whom joined the bandwagon simply because it was new and fashionable, tire and the opponents, although investing less energy in the debate, relax, feeling that the matter has been finally laid to rest. At this stage the mere mention of the subject leads to blank stares or derisive laughter. But, from the trough of this wave, the proponents, strengthened and refined by the opposition, rethink their arguments, the science is consolidated and the field slowly begins to grow. Eventually young physicians, unaware of the original controversy accept the development without prejudice and, meanwhile, natural mortality finally takes care of the opposition. Oxygen therapy under hyperbaric conditions is going through this evolution and is gaining momentum as acceptance is growing throughout the world often driven by patients and their relatives. However major initiatives are needed, especially to allow the proper treatment of diseases of the nervous system. At the moment, despite the comprehensive information and experience derived from the therapy of decompression sickness affecting the brain and spinal cord, there is wide disagreement about neurological indications, even among the hyperbaric oxygen community. Major developments have occurred in diagnostic medicine, such as magnetic resonance imaging, which constantly point to hypoxia and the increased tissue water content of edema as a critical component in many diseases, from the exotic territory of the brain to the mundane problem of varicose ulceration. The presence of hemoglobin is an obvious reminder that oxygen is poorly soluble in water. Strictly, oxygen therapy includes all of the clinical situations where the partial pressure of oxygen is raised above 0.2 atm abs., the partial pressure of oxygen in air. Obviously the advocacy of the delivery of oxygen under hyperbaric conditions is a special case and confronts practitioners with the uncomfortable possibility that they are not using oxygen properly. It is not difficult to understand the resentment that this may generate, after all, oxygen is available in every hospital and has been used for many years. Unfortunately, it means a return to basics and as Epictatus stated in the 3rd century BC;
It is impossible to learn what we think we already know.
The arguments against oxygen therapy must be met - toxicity is easily dealt with - because the dose time limits of hyperbaric oxygen therapy are very well established and include data from millions of man hours of pure oxygen breathing in military diving. So are the minor barometric problems, such as clearing the middle ear. Cost, however, can be a major stumbling block. Of course, no one can surely deny that intensive care in a large multiplace chamber is bound to be expensive in terms of personnel and equipment but the use of a pressurized room does not add much to the cost of such interventions. However, we need to separate this high-technology approach from the simple low-pressure mundane oxygen protocols required to assist in wound care. Of course, some hyperbaric physicians will argue that charges must be high to cover costs in view of the small number of patients treated. However there is no shortage of patients who can benefit; simple management of varicose ulcers costs the NHS about 2% of the NHS budget - £800 million a year. It is in these circumstances that cost-benefit arguments are used by health care professionals, despite the fact that many of us feel that it is not our remit to be concerned about finance, but to do the best for our patients. Although attempts have been made to make hyperbaric medicine a speciality, it is not and every physician and surgeon should be capable of prescribing this treatment and supervising its application, just as overall responsibility can be retained in other therapies. What is obvious is that the proper place of hyperbaric oxygen therapy is in emergency and acute care, for so long the Cinderella of Medicine. What can be done to secure change? Today patients are better informed and we must look to the education of both physician and patient to confront attitudes that too long have gone unchallenged. Giving more oxygen is not alternative medicine, it is sound science and commonsense. There is no substitute for oxygen and hyperbaric medicine must be included in the core curriculum of our medical schools.
For PDF version of the HYPERBARIC OXYGEN TREATMENT : THE LAST FRONTIER click here...
Sponsored links:











